When I left you last we had just returned from Rome and were heading into what turned out to be a lovely, if busy Christmas, with lots of family down and a lot of fun was had by us all. As usual Jo was doing too much, but she wouldn’t have had it any other way, cooking for 10 on Christmas Day and 11 on Boxing Day.

Following Christmas Jo’s wheeziness and cough started to worsen, so by the time New Year’s Eve came round she was really feeling quite unwell. We were due to visit the Hospice for an introductory session in the morning and so decided not to ring anyone but wait to see them and ask what we could do to improve the coughing and breathlessness.
So we arrived at the Hospice and was greeted by our Clinical Care nurse, who immediately noticed Jo wasn’t very well and after an initial introduction said she would get one of their doctors to see us, who immediately told us to go to the accident and emergency department as it looked like Jo had a chest infection.
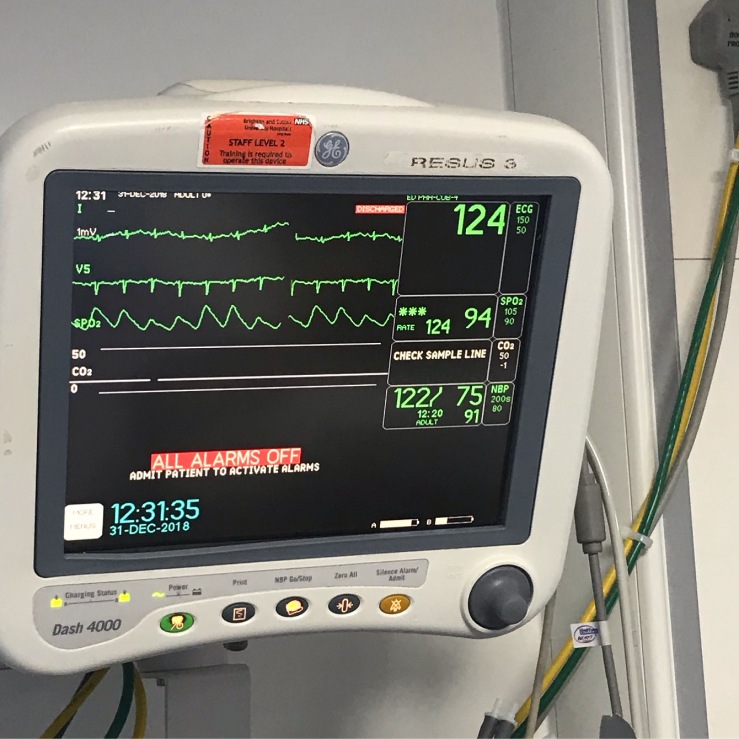
So off to A&E we went where we were seen straight away (one of the few perks of being a cancer patient) and they diagnosed Jo with pneumonia in both lungs. Jo was admitted and placed in a respiratory ward with 5 older women, given intravenous antibiotics and oxygen to help with her breathing. Also her heart rate was very high (120-130) and had been for the last few days (as seen on her apple watch data) which was another sign of pneumonia. So Jo saw in the New Year in hospital and I managed to briefly get to the pub with a couple of friends, but it wasn’t the New Year we had hoped.
After two nights in the ward and Jo unable to sleep, due to the noise of the other patients and her discomfort, we managed to get her transferred to the private hospital we had been using for Chemo and back under the care of our oncologist.

The Montefiore in Hove is a lovely hospital, more like a hotel and we immediately felt we were receiving much more focussed care and things started to happen. The next morning our oncologist and the matron came to visit and arranged CT scans and a chest x-ray. They increased Jo’s painkillers so she was in less pain and the nurses were very attentive and did all they could to help her.
Later that afternoon the oncologist was back to advise they were going to drain the right lung in the morning as the pleural effusion had got bigger. Also he was arranging a ECHO heart scan to see what was going on there, as the heart rate was still very high.
Next morning Jo went for the lung drain before I arrived at the hospital and when she arrived back on the ward she was very drowsy. I had presumed they had given her a sedative for the drain to be put in, but the nurse said it was just local anaesthetic. She just didn’t seem right.
As the morning went on, she was still drowsy and when the time for the ECHO to take place, I was starting to get worried. I waited nervously in her room for her to return and as time went on my anxiety was building, eventually, the matron came in and I knew something was wrong. She sat down beside me and explained they had found a lot of fluid around her heart which was stopping her heart from pumping properly and she was very seriously ill. They were arranging an ambulance to take her to the Royal Sussex County hospital a few miles away in Brighton where she would get rushed in to the Cardiology unit. I asked whether I should get the family together and was told I should.
I rushed to the County in my car, beating the ambulance, while trying to contact my children, Jo’s Mum and her brother (who was on holiday in Prague). A few of our closest friends helped get the kids and Jo’s Mum to the hospital which is 40 minutes from our home.
When the ambulance arrived we were rushed into a chaotic and overcrowded resus waiting area, where we anxiously waited for a bay to become available. The matron from the Montefiore had dropped everything and come with Jo in the ambulance and I could tell she was anxious about the wait. Luckily the cardiology team came down and whisked Jo straight up to their operating room to perform a drain of the fluid around her heart.
Crisis had been averted for now, but it became clear from talking to the doctors and the matron that Jo had been close to death over those previous hours. Jo was admitted to the Cardiac centre and put on various monitors. Her heart rate was still high and she was on Oxygen in the emergency unit but she was stable. The lung drain had taken out an impressive 2 litres of fluid over the day and they had drained a sizeable 850ml from around her heart.
The nurses in the Sussex Cardiac Centre were exceptional, they monitored her closely and were great to me, even allowing me to stay in a spare bed in the unit.
The next morning saw a visit from our Oncologist and the devastating news that I half expected but Jo didn’t really see coming, that the cause of the fluid was the underlying cancer, which seemed to love the shiny surfaces in the body, the linings such as the skin, the pleural membrane (around the lungs), the lining of the Pericardium (around the heart) and it was also now seen in the linings of the abdomen. Whatever they had done to try and stop the Cancer, it had been at least one step ahead and it had got to the stage where it was now sadly out of control. He advised that Jo was probably unlikely to be fit enough to continue chemotherapy and certainly not in the near future and that we should prepare for the worst.
We had agreed we wouldn’t ask how long she might have left until there was no hope of at least delaying it but that time had arrived, so I asked him how long we were looking at and he advised days, maybe weeks. Tears began to flow from both myself and Jo and for a short while I couldn’t speak. I just held her hand and gave her a hug.
The oncologist then spoke about getting us to the hospice as it was unlikely that Jo would be well enough to go home, but with some time in the hospice and if they could stabilise her condition maybe she could. She would stay in the County for now while they monitored her condition and while the drains remained in place but hopefully in a couple of days they would be able to get her out as long as the fluid around the heart stopped increasing.
We also agreed to a ‘Do not resuscitate’ agreement, so in the event of her heart stopping, no action would be taken.
Jo to my surprise didn’t fall apart, she accepted the situation, even though it was a great shock to her, she showed courage and bravery that I didn’t know she possessed. In fact I was the one struggling to come to terms with the prognosis, even though I suspected it would come. She shrugged and said well it could have been worse she could already be dead, at least she has a little time left.
The next couple of days saw Jo improving her heart rate dropped to the 90’s which is still high but nothing compared to the previous week, she managed to get some sleep and eat. The nurses again were great on the ward and I have the utmost praise for them, they let me stay with her throughout, which was something they didn’t let anyone else do, but they understood that we didn’t have much time to be together.
On the Monday we got the good news that a bed was available in the hospice and both the lung and heart drains were removed, so a week after arriving at the hospice rather unwell, we were back there and actually feeling much better.
Jo has always been determined since her incurable diagnosis, that she wanted to die at home, so we immediately started to try and persuade the nurses and doctor at the hospice that she would be better off at home and after examining her they agreed. So about an hour after arriving at the hospice we were on our way home.
We have had a few days at home now and we have been visited by the district nurse and the hospice community care nurse and feel more confident about getting Jo’s final wish. I have spent a fair amount of time getting the relevant painkillers and other drugs to the house for Jo and we are trying to find a balance of drugs to keep her out of pain but not too drowsy, which hasn’t been easy. She is still quite out of breath and her skins mets are sore but we hope to get all that under control as best we can. I am becoming a pharmacist in my spare time, to go with my oncologist and breast surgeon specialties that I have done over the previous 3 years.
We have managed to get Jo out to her favourite restaurant for dinner with our son and best friends which was something she really wanted to do.

We have also had to start looking at the practical things, I need to know her wishes, what she wants to gift, how she wants her funeral etc, tough discussions but necessary and one way we can make these days or weeks a benefit. I have a list created and hopefully will do her proud.
Between the Hospice, District Nurses, GP and paramedics (if required) we hope to keep her out of hospital and get her final wish, but we hope there is no rush. It has been great having her home, where she belongs and for a while it didn’t look like it would happen, but that is testament to her strength and courage, she is an amazing woman and I am very proud to call her my wife.

Having travelled a similar path to you I feel devastated to read your news but very familiar with the situation. If I can help in any way please ask. Even just to sound off against.
LikeLiked by 1 person
Thanks Simon. Much appreciated.
LikeLike
Thank you so much for this very moving update you are all on our minds constantly I pray that Jo is settled now she is at home with all her loved ones around her ..god bless you All ❤️❤️ With much love JJ and Frances xxxx
LikeLiked by 1 person
Thanks Fran x
LikeLike
Beautifully written and I could feel you keeping it together throughout the post. It’s good to hear about another womsn whose fighting spirit refuses to give in and who wants to be in her family’s arms rather than caught in a series of hospitalizations or hospice. Death comes to all living with metastatic disease – I think we are all happy to see each day no matter what that day brings. It brings breath and our breathing brings in the love around us and both love and oxygen are critical for our lives to continue in some meaningful way. Without you, Jo wouldn’t have one key to live on and fight for another day. Thank you. I will let my husband read your post if he will, since he cannot accept the fact that I will, too, not live forever and the scare we had over Xmas wasn’t just a scare but a wake up call he can’t answer.
LikeLike
Thanks Ilene for your kind words and good luck to you and your husband.
LikeLiked by 1 person
Thinking of you all at this very difficult time & praying that Jo is in as little discomfort as possible.
With love. Gill & Mike xx
LikeLiked by 1 person
Thank you x
LikeLike
What a hard blog to write Kieran ……. it must have been done with a heavy heart! But thank you for doing it. Glad Jo is able to be at home with you all savouring the time she has left. You are doing such an amazing job looking after Jo and she must take great comfort from that. Loving thoughts to you all
LikeLiked by 1 person
Thanks Fiona x
LikeLike
An incredibly moving update Kieran. You are an inspiration to us all sharing these experiences. Glad Jo is able to be at home with you all. Our thoughts are with you.
LikeLiked by 1 person
Thanks David.
LikeLike
Thinking of you, Jo and the family.
Stu & J x
LikeLiked by 1 person
Thanks Stu. Hope you are all well
LikeLike
I can only echo the sentiments already posted here. Your courage is an inspiration.
X
LikeLiked by 1 person